
The protocol for the 'Conventional ventilation or ECMO for Severe Adult Respiratory failure (CESAR) Trial was published in 2006. Uncertainty about the effectiveness of referral to an ECMO centre led to a trial to assess the costs and effectiveness of the new form of care funded by the NHS Health Technology Assessment programme. In addition to the costs of alternative forms of care, the economic choice depends on the value of the outcome gained. Thus the health service costs and the household costs might fall at any stage of the treatment and recovery, and in many different forms. Finally, if there is increased survival to discharge from hospital, then there will be more use of services in primary and community care, and requirement for help for recovering people at home. In addition, because appropriate care is provided in relatively few centres, the location of care and need for specialist transport for patients also affects the costs of care. Differences in lengths of stay and types of care received by patients following either clinical pathway may result in different statistical distributions of cost for inpatient care. However, conventional treatment for severe respiratory failure is also one of the more costly forms of care in any health system. Given the high cost of treatment, ECMO is considered an expensive technology for many funding systems. However, considerable improvements have also been reported in survival rates of conventionally treated patients with severe respiratory failure.
Many centres in the world use ECMO technology and have reported survival rates in excess of 50% in uncontrolled observational studies of patient outcomes. It soon became clear however, that although ECMO was effective and cost effective compared to conventional ventilation in newborns, the evidence was much less clear for the adult population. The early reports of the use of ECMO in adult with severe respiratory failure were enthusiastic.

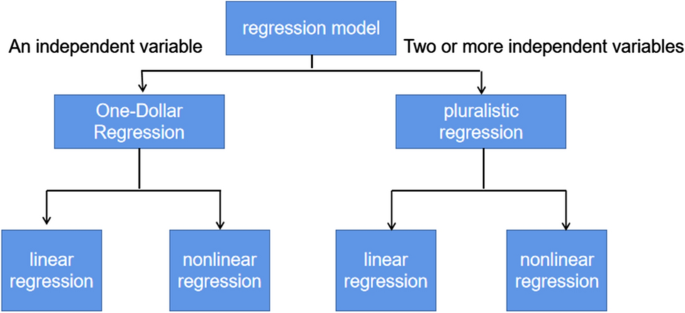
The technique involves placing patients on a life support circuit with a membrane oxygenator to temporarily take over the gas exchange function of e lung thereby allowing the lungs to rest and recover.
#Economic data analysis methods registration#
The CESAR trial registration number is ISRCTN47279827.Įxtracorporeal Membrane Oxygenation (ECMO) was introduced into treatment of severe but potentially reversible respiratory failure in the 1970s. In our view it is important to record our methods in detail and present them before publication of the results of the trial so that a record of detail not normally found in the final trial reports can be made available in the public domain. Probabilities of cost effectiveness given different funding thresholds will be estimated. Uncertainty will also be expressed in analysis of individual patient data. Sensitivity analysis is planned to vary assumptions about transport costs and method of costing intensive care. Cost utility analysis is based on quality adjusted life years gained based on the Euroqol EQ-5D at 6 months. Cost effectiveness analysis uses the outcome: survival without severe disability. Other unit costs are based on published NHS tariffs. Unit costs of hospital intensive care resources are based on parallel research on cost functions in UK NHS intensive care units. Resource use data are collected from clinical report forms and through follow up interviews with patients. Resources used by patients in the trial are identified.

The objectives of the economic evaluation are to compare the costs of a policy of referral for ECMO with those of conventional treatment to assess cost-effectiveness and the cost-utility at 6 months follow-up and to assess the cost-utility over a predicted lifetime. The protocol and funding for the CESAR trial included plans for economic data collection and analysis. A multi-centre randomised controlled trial (CESAR) was funded in the UK to compare care including ECMO with conventional intensive care management. Extracorporeal Membrane Oxygenation (ECMO) is a technology used in treatment of patients with severe but potentially reversible respiratory failure.


 0 kommentar(er)
0 kommentar(er)
